Arthritis is one of the principal causes of disability worldwide. For those afflicted with it, arthritis limits everyday activities and reduces quality of life. Today, in the United States alone, there are 52.5 million adults diagnosed with arthritis.
Women have a higher risk than men, and the risk increases with age. Family history, obesity, joint injuries, joint infections, and lifestyle play roles in the development of arthritis. Current treatments for arthritis include physical therapy, medications, and surgery for severe arthritis cases.
Medications can help control arthritis symptoms, but long-term use can do more harm than good. Studies now show cannabis may be a safer alternative treatment for arthritis.
Understanding Arthritis
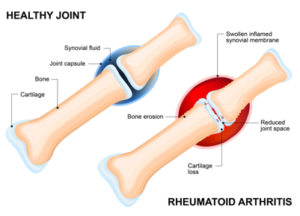
Arthritis is not a single disease, but rather a class of more than 100 disorders that affect the joints. Joints have a synovial membrane covering them which houses nourishing blood vessels. This membrane produces a sticky liquid called synovial fluid, which lubricates the cartilage covering the surface of the bones to facilitate easy, pain-free movement. Firm, resilient, flexible, and smooth – cartilage acts like a cushion absorbing impact and shock caused by movement.
Pathophysiology of Arthritis
Triggers, such as genetic predisposition, lifestyle (smoking, diet, occupation), infections, and autoimmune disorders can change this normal joint structure, leading to various arthritis symptoms including painful joints, stiffness, swelling, tenderness, and even deformities.
These triggers cause a cascade of inflammatory effects1. Synovial cells increase in size and quantity, eventually signaling an increase in mononuclear cells (lymphocytes and monocytes), and causing the proliferation of T-cells. Once activated, these T-cells secrete cytokines and chemokines which increase inflammation to fight the antigen.
Cytokines activate another lymphocyte (B-cells) increasing the production of antibodies and increasing inflammation. Cytokines also increase mast cells which release histamines to attack antigens. In rheumatoid arthritis, other types of cells – fibroblasts, osteoclasts, and macrophages – also increase, further worsening the inflammatory process. This causes thickening, swelling, inflammation of the synovium, and a release of destructive enzymes.
Pannus formation2, an abnormal layer of tissue3 which covers the bone surface and the articular cartilage, is common in rheumatoid arthritis and osteoarthritis. When inflammation occurs, and cytokine levels rise, blood vessels in the synovial membrane open causing more blood flow and faster synovial cell growth. This cell growth leads to increased thickness of the synovium, unevenness, and roughness of the surface. The synovium expands into other areas to accommodate for its increased thickness. Pannus cells migrate to this area covering the surfaces while secreting excess fluid and enzymes, degrading cartilage and bone. The high number of osteoclasts in the pannus layer secrete proteins and produce an acid which destroys bones leading to increased pain, decreased joint movement, and development deformities.
Current Treatments for Arthritis
Medications used to treat arthritis can relieve symptoms and improve joint function:
- Analgesics for pain control.
- NSAIDs for pain and inflammation.
- DMARDs for an overactive immune system.
- Corticosteroids, also for an overactive immune system.
But these arthritis medications may have adverse side effects:
- NSAIDs cause GI problems like ulcers and increase the risk of heart attack and strokes.
- Corticosteroids cause cataracts, increased appetite, weight gain, increased blood sugar levels, high blood pressure, and risk of blood loss.
- DMARDs cause GI upset, headache, nausea, fatigue, and increased risk for infection.
- Analgesics are highly addictive, cause liver damage, and even fatal overdose.
Long-term use of these arthritis medications can cause serious complications4 like damage to the liver, kidneys, eyes, lungs, heart, GI, and neuropathy.
Cannabis: An Alternative Treatment for Arthritis
The endocannabinoid system5 (ECS), although found throughout the body, is predominantly located in the central and peripheral nervous systems. ECS receptors are found in organs, glands, connective tissues, and the immune system. Their primary function is to promote homeostasis in the body. However, receptors also play a role in pain sensation, inflammation, mood, memory and learning processes, appetite, locomotion, and other physiological processes.
The ECS has two primary receptors6 – CB1 and CB2. The nervous systems, organs, glands, and connective tissues mostly have CB1 receptors; while the immune system and peripheral system predominantly have CB2 receptors. CB1 receptors play a vital role in pain sensation, mood, appetite, sleep, and memory, and produce the psychoactive effects of cannabis. Whereas, CB2 receptors affect the inflammatory process and suppress the immune system.
The ECS responds to endocannabinoids (cannabinoids created within the body). However, they are produced only when needed, and their effects are localized and short-lived since they are easily degraded by enzymes.
The ECS is known to be essential for homeostasis of the body, and many studies have been conducted to determine if phytocannabinoids (cannabinoids from cannabis), working in conjunction with endocannabinoids, can be more effective than conventional treatment options for arthritis.
Cannabinoids Control and Relieve Pain
THC, the most common cannabinoid, controls how pain is perceived by the brain. In one study7, researchers applied capsaicin topically on 12 healthy male volunteers. Capsaicin instantly produced a burning sensation in the immediate and surrounding areas. Stimulation of the area increased the sensation of pain.
During four sessions, THC and a placebo were given to the participants. Results showed THC decreased pain caused by the capsaicin and the stimulus. Also, MRI scans showed altered functional activities in some parts of the brain, proving the introduction of THC influences the brain’s response to pain stimulus.
CBD, a non-psychoactive cannabinoid, can also alter pain perception by influencing the function of the TRPV-1 receptor8, commonly known as vanilloid receptor 1, which detects and regulates changes in body temperature and produces the sensation of heat and pain. CBD binds to these receptors, stimulating them to hasten desensitization, thus causing a reduction of pain.
CBD Prolongs the Effects of Endocannabinoids
Anandamide, an endocannabinoid, is a neurotransmitter involved in many physiological processes including pain perception. Stimulus, like pain, allows the release of anandamide, activating the peripheral CB1 receptors, and controlling the pain signals9 sent to the brain. Unfortunately, enzymes break down endocannabinoids quickly.
CBD can suppress the action of enzymes10. By inhibiting certain enzymes, cellular uptake and degradation of anandamide are reduced allowing it to circulate through the body longer.
Cannabinoids Reduce Inflammation
Although joint inflammation is common with arthritis, the severity varies depending on the type of arthritis. Joint inflammation in rheumatoid arthritis is symmetrical, more severe, and affects multiple joints; whereas osteoarthritis affects only weight-bearing joints and is not as severe.
A study11 conducted on the effects of THC and CBD on microglial cells showed both cannabinoids have multiple ways of reducing inflammation12:
- THC and CBD curb the production of cytokines.
- THC and CBD repress STAT1, a key element in the pro-inflammatory process.
- CBD suppresses a signaling pathway regulating pro-inflammatory genes and regulating the body’s response to infection and stress. Suppressing this pathway reduces inflammation.
- CBD boosts the activity of STAT3, which plays a role in homeostasis and anti-inflammatory processes.
- CBD suppresses enzymes, increasing endocannabinoid concentration.
Other ways13 CBD helps reduce inflammation:
- Stimulating the TRPV-1 receptors involved in the inflammatory process producing analgesic and anti-inflammatory effects14.
- Stimulating the adenosine receptors producing anti-inflammatory effects15.
Studies on Cannabinoids as a Treatment for Arthritis
Other studies prove cannabinoids are an effective treatment for arthritis:
- In a double-blind study16, 58 patients suffering from rheumatoid arthritis were given either cannabis or a placebo. Of the 58 patients, 31 received cannabis, while 27 were given placebo treatments. Over the course of five weeks, they were given oral spray at night and assessments were taken each morning of their pain, morning stiffness, and quality of sleep. Those who received cannabis reported marked improvement in their symptoms as compared to those who received a placebo.
- CBD is an effective anti-inflammatory and anti-arthritis drug according to this study17. Mice, immunized with type II collagen to elicit acute collagen-induced arthritis symptoms, were given CBD orally or through injections. The results showed that CBD effectively blocked the progression of arthritis, and enabled clinical improvement in the mice. Studying their lymph nodes showed a significant decrease in type II collagen. Examining the knee synovial cells revealed a reduction of tumor necrosis. CBD proved to be equally effective whether administered orally or by injection.
- Another study18 done on mice to investigate the effectiveness of CBD on pain and inflammation also showed positive results. Carrageenan, a substance from seaweed, was injected into the soles of mice, resulting in pain and inflammation of the area. After the onset of the symptoms, CBD was then given to the mice orally for three days. At the end of the study, the mice all displayed a reduction in the levels of previous assessments.
THC and CBD are two of the most studied cannabinoids for arthritis treatment. While THC directly acts on the CB1 receptors to produce the anti-inflammatory effects, it also generates the “high” associated with cannabis use.
CBD works a little differently though. CBD does not directly stimulate the CB receptors to produce its beneficial effects. Instead, it stimulates other receptors responsible for pain and inflammation. Furthermore, CBD regulates the psychoactive effects of THC19 by suppressing and deactivating the enzyme which metabolizes THC.
CBD, as proven by several studies, is an effective analgesic and anti-inflammatory medication for arthritis. Additionally, CBD’s antioxidant properties20 and lack of significant side effects21 could make it a safer choice than other medicines used to treat arthritis.
References:
1 Joint Pain Expert, Rheumatoid Arthritis athology.
http://www.joint-pain-expert.net/rheumatoid-arthritis-pathology.html
2 Furuzawa-Carballeda J, et al. July and August 2008.
The National Center for Biotechnology Information, Osteoarthritis and rheumatoid arthritis pannus have similar qualitative metabolic characteristics and pro-inflammatory cytokine response.
https://www.ncbi.nlm.nih.gov/pubmed/18799084
3 Judith Frank, MD. November 17, 2015.
Arthritis Health, What is Pannus?
http://www.arthritis-health.com/types/rheumatoid/what-pannus
4 WebMD, Rheumatoid Arthritis Drug Guide.
http://www.webmd.com/rheumatoid-arthritis/guide/rheumatoid-arthritis-medications#1
5 Dustin Sulak, DO. February 2015.
NORML, Introduction to the Endocannabinoid System.
http://norml.org/library/item/introduction-to-the-endocannabinoid-system
6 Leaf Science,
CB1/CB2 Receptors.
http://www.leafscience.com/endocannabinoid-system/works/cb1-cb2-receptors/
7 Michael C. Lee. January 2013.
Science Direct, Amygdala activity contributes to the dissociative effect of cannabis on pain perception.
http://www.sciencedirect.com/science/article/pii/S0304395912005453
8 Barbara Costa, et al. August 16, 2001.
The National Center for Biotechnology Information, Vanilloid TRPV1 receptor mediates the antihyperalgesic effect of the nonpsychoactive cannabinoid, cannabidiol, in a rat model of acute inflammation.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1575333/
9 Clapper, JR, et al. September 19, 2010.
The National Center for Biotechnology Information, Anandamide suppresses pain initiation through a peripheral endocannabinoid mechanism.
https://www.ncbi.nlm.nih.gov/pubmed/20852626
10 Project CBD, How CBD Works.
https://www.projectcbd.org/how-cbd-works
11 Ewa Kocela, et al. November 12, 2009.
The National Center for Biotechnology Information, Cannabinoids Delta(9)-tetrahydrocannabinol and cannabidiol differentially inhibit the lipopolysaccharide-activated NF-kappaB and interferon-beta/STAT proinflammatory pathways in BV-2 microglial cells. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2804319/
12 Kozela E, et al. January 15, 2010.
The National Center for Biotechnology Information, Cannabinoids Delta(9)-tetrahydrocannabinol and cannabidiol differentially inhibit the lipopolysaccharide-activated NF-kappaB and interferon-beta/STAT proinflammatory pathways in BV-2 microglial cells.
https://www.ncbi.nlm.nih.gov/pubmed/19910459
13 Project CBD,
How CBD Works.
https://www.projectcbd.org/how-cbd-works
14 Fumio Tsuji and Hiroyuki Aono. August 2012.
The National Center for Biotechnology Information, Role of Transient Receptor Potential Vanilloid 1 in Inflammation and Autoimmune Diseases.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3763671/
15 Sullivan, GW. November 2003.
The National Center for Biotechnology Information, Adenosine A2A receptor agonists as anti-inflammatory agents.
https://www.ncbi.nlm.nih.gov/pubmed/14758770
16 DR Blake, et al. November 9, 2005.
The National Center for Biotechnology Information, Preliminary assessment of the efficacy, tolerability and safety of a cannabis-based medicine (Sativex) in the treatment of pain caused by rheumatoid arthritis.
https://www.ncbi.nlm.nih.gov/pubmed/16282192
17 Malfait AM, et al. June 2, 2000.
Proceedings of the National Academy of Sciences, The nonpsychoactive cannabis constituent cannabidiol is an oral anti-arthritic therapeutic in murine collagen-induced arthritis.
http://www.pnas.org/content/97/17/9561.full
18 Barbara Costa, et al. February 12, 2004.
Springer Link, Oral anti-inflammatory activity of cannabidiol, a non-psychoactive constituent of cannabis, in acute carrageenan-induced inflammation in the rat paw.
http://link.springer.com/article/10.1007/s00210-004-0871-3#page-2
19 Adrian Devitt-Lee. September 17, 2015.
Alternet, CBD-Drug Interactions: The Role of Cytochrome P450.
http://www.alternet.org/drugs/cbd-drug-interactions-role-cytochrome-p450
20 AJ Hampson, et al. July 7, 1998.
The National Center for Biotechnology Information, Cannabidiol and (−)Δ9-tetrahydrocannabinol are neuroprotective antioxidants.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC20965/
21 Bergamaschi MM, et al. September 1, 2011.
The National Center for Biotechnology Information, Safety and side effects of cannabidiol, a Cannabis sativa constituent.
https://www.ncbi.nlm.nih.gov/pubmed/22129319


Leave a Reply
You must be logged in to post a comment.